Article
Why virtual wards? And how do EPRs help?
NHS England published the “Delivery plan for recovering urgent and emergency care services” earlier this year, outlining NHS England’s commitment to the public to improve waiting times, tackle elective recovery and improve patient experience.
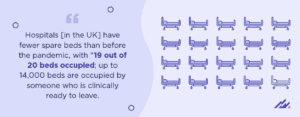
Hospital occupancy levels are now at record levels and patient “flow” is an issue for many hospitals. Covid-19 is still with us, alongside the seasonal pressures of flu, coupled with more than 7M people waiting longer for elective treatments. The pressures on the health service are greater than ever before.
Hospitals have fewer spare beds than before the pandemic, with “19 out of 20 beds occupied; up to 14,000 beds are occupied by someone who is clinically ready to leave.” Consequently, beds are effectively blocked, and patients are having to spend longer in A&E as well as waiting longer for ambulances as there is simply not the capacity to admit them.
 Expanding and optimising patient care outside hospital
Expanding and optimising patient care outside hospital
NHS England’s plan outlines many initiatives to improve the bottlenecks contributing to bed blocking. One key component is expanded provision of virtual wards, so that people can be better supported at home for their physical and mental health needs, and to avoid unnecessary readmissions to hospital. The pandemic highlighted how it was possible to adopt new care delivery models and ways of working. Clinical evidence is also growing to support the benefits of such virtual wards.
What are virtual wards?
Virtual wards act like a hospital at home. Patients can be physically discharged to their home environment, but their care and clinical responsibility remains with the hospital until clinical discharge. This is reducing length of stay, freeing up hospital beds and improving patient experience of care. Virtual wards also reduce the downside of extended hospital admissions, such as hospital-acquired infections and other complications related to reduced activity and institutionalisation. Virtual wards have been around for some time but historically have been focused on specific conditions. The experience of managing patients from afar during the pandemic coupled with both clinicians’ and patients’ adoption and acceptance of technology has enabled acceleration of the virtual ward concept for both early discharge following elective procedures as well as supported discharge following emergency admissions. Over the intense Covid-19 period, virtual wards were expanded to monitor sick patients at home when bed availability was at its lowest and hence enabled many patients to avoid hospital admission whilst still being under regular clinical review.
How do virtual wards work?
Patients are treated with a regular cadence of phone calls, assessments and face-to-face visits depending on their needs. Some conditions also warrant physiological monitoring at home, with pulse oximetry and blood pressure being some of the commonest measurements. Patients are carefully assessed for their suitability for an early supported discharge. The key aim is to get people home more quickly. The support from the virtual ward staff gives the patient and their family the confidence to get them home knowing they are still being monitored and that the regular check-in creates opportunity for any concerns to be heard.
What is the link with EPR?
As part of the identification of patients suitable for continuing care in a virtual ward, the clinical data in the EPR is a critical resource. It enables the hospital-based assessors to review key data that will inform the patients’ suitability—this starts with visibility of the patients’ estimated discharge date and any factors that may threaten that date or prevent an earlier discharge. Other EPR data both from a clinical aspect but also from a social aspect is critical, such as baseline function and whether the patient lives alone, has support already, etc.
More importantly, utilisation of the same single patient record within the EPR once the patient is discharged from hospital and admitted to the virtual ward ensures consistency of documentation and compliance with standard protocols. A virtual ward tracking board provides an overview of patients currently “admitted” and the progress and activities planned. It also highlights any potential deteriorations or concerns as wells as gaps in care or clinical documentation, enabling staff to prioritise their reviews of patients under their care.
Staff members can quickly find the information they need and can review serial assessments so that any changes in patients’ conditions—both objective and subjective—can be assessed in the context of previous data points from the recent hospital visit. This enables staff that may not have met the patient before to quickly ascertain if changes are concerning. When home visits are required, staff can access the same data remotely from a laptop, saving staff the need to “return to base” to review or update records.
Altera Digital Health clients that have configured virtual wards within their EPRs have benefitted from repurposing existing inpatient documentation and forms so that there is consistency across the care settings and a new admission from hospital to a virtual ward will already have elements of a plan in place, which can then be reviewed and updated. Staff have easy access to historical blood results and details of microbiological infections as well as the medication changes that may have occurred in hospital should further optimisation be required.
For those that need ongoing physiological monitoring, multiple approaches can be deployed. Some patients may go home with equipment they can use to record their observations and report back to the clinical team at the regular check-ins. Others have devices connected so that remote visibility of these observations is scrutinised by the clinical team and any anomalies can be escalated for urgent review. The technology for this at home monitoring has been designed to be less and less complex so that patients are not burdened with issues setting up connections. We are working with our clients to enable this data to flow directly into the EPR, having first been clinically reviewed to reduce the need for transcription.
When the patient has recovered and the virtual oversight is no longer needed, the EPR data collected can feed into a virtual ward discharge summary that can utilise existing processes for this formal handover of care to the GP.
If a patient’s health deteriorates, their contact with the virtual ward and the links to the discharging hospital team facilitate the readmission to hospital. This saves patients from protracted emergency admission processes where their previous histories are not necessarily at hand.
An approach welcomed by patients
Early analysis of patients’ views of virtual wards has been extremely positive. One benefit that nursing staff working in these remote wards have unexpectedly reported is that they get to know their patients far better than they might have done on busy wards – whilst they may not be physically next to the patient, the privacy the patient has in their own home and the frequent one-on-one conversations help patients to open up and discuss more than they might have when only separated from other patients and staff by flimsy curtain on a ward.
Individual patient stories often highlight the real differences this service enables. One patient who has had recurrent hospital admissions for infective exacerbations of COPD said that he felt confident to reduce his oxygen dependence sooner and come off it altogether much faster compared to previous hospital admissions of the past. His early discharge supported by the virtual ward team meant he was less nervous about weaning himself off the oxygen and hence was able to mobilise and recover faster—all within the comfort of his own surroundings.
One study shows that in one acute hospital, 200 bed days are saved per month by having a 40-bed virtual ward that provides care at home. The availability of suitable technology to enable home-based monitoring, with the facilitation of consistent data review and collation for patients on virtual wards, enhances the delivery of safe consistent care. The government’s target to increase utilisation of virtual wards from 65% to 80% and enable 50,000 admissions a month will require significant clinical team recruitment.
For trusts with a flexible EPR, many of the technology requirements can be harnessed to support clinical oversight, documentation, and reporting. Provision and deployment of home monitoring devices and connections are not required for all patients who could benefit from virtual wards, but early indication shows that integration with these devices would add further benefit for staff and patients.
The utilisation of existing EPR technology to support the virtual ward initiative will be key to successful implementation of this approach to reduce length of stay and avoid admission or re-admission. The single repository for clinical data will also enable analysis of the patient cohorts benefitting from this service so that it can be further optimised for safety and efficiency and expanded to a wider range of eligible conditions and needs.
When we consider the future of healthcare, we know there’s a lot of work to be done. We know healthcare IT needs to be better, and at Altera, we see the path towards better outcomes. Now, the journey upwards begins, and together we will achieve more every day. To learn more about how our health technology offerings can help meet and exceed your organisation’s needs, go here.